With the introduction of the new SIRS from the start of April, aged care providers have a number of additional obligations around reporting incidents classed as abuse or neglect.
The scheme however goes beyond reporting, requiring that providers have in place organisation-wide systems and process to identify, record, manage incidents.
And furthermore, that they use incident data to drive continuous improvement.
Intended to complement the Aged Care Quality & Safety Standards, in particular, Standard Six: Feedback and Complaints and Standard Eight: Organisational Governance, the introduction of SIRS is not just a separate mechanism to ensure quality in aged care, but an imperative to begin to break down silos in data and use these insights to implement and monitor improvements.
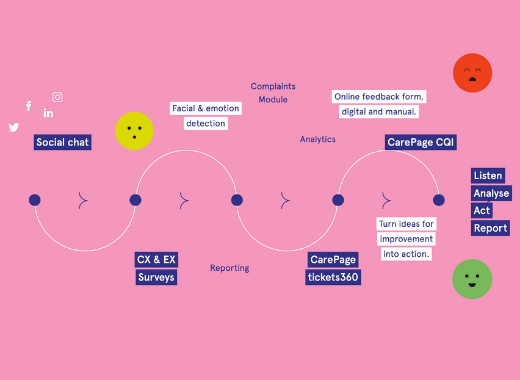
In order to impact the overall quality of aged care, providers need to have in place systems that will allow them to link, report, analyse and use data across all three important areas feedback, complaints and incidents.
Are your systems ready to do this?
What is the Serious Incident Response Scheme (SIRS)?
The SIRS is a new initiative that aims to combat cases of abuse in Australian aged care facilities.
From the start of April 2021, the SIRS will hold aged care providers to higher standards of reporting abuses and require providers to have effective management systems in place.
According to the Aged Care Quality and Safety Commission website, “SIRS sets new arrangements for approved providers of residential aged care to manage and take reasonable action to prevent incidents with a focus on the safety, health, well-being and quality of life of aged care consumers.”
Under SIRS, providers will have to report a wider range of incidents to the Commission within certain time frames depending on the severity of the incident and its impact on the resident.
Approved providers will be required to have in place an effective incident management system and to use this to continuously improve the management and prevention of incidents. Under SIRS, approved providers will be required to report a broader range of incidents to the Commission than previous arrangements. Incidents must be reported within set time frames depending on the level of impact to the care recipient.
From April 1, all incidents falling under ‘Priority 1’ designation must be reported within 24 hours of that incident becoming known. From October 1, other incidents falling under ‘Priority 2’ must be reported within 30 days.
“‘Priority 1’ incidents must be reported to the Commission within 24 hours of becoming aware of the incident. This is a reportable incident where the incident has caused, or could reasonably have caused, a care recipient physical or psychological injury or discomfort that requires medical or psychological treatment to resolve,” says the Commission website
“‘Priority 2’ incidents must be reported to the Commission within 30 days of becoming aware of the incident. This includes all other reportable incidents that do not meet the criteria for a ‘Priority 1’ incident.”
According to the Commission website, reportable incidents include:
- Unreasonable use of force – for example, hitting, pushing, shoving, or rough handling.
- Unlawful sexual contact or inappropriate sexual conduct – such as sexual threats or stalking, or sexual activities without consent.
- Psychological or emotional abuse – such as yelling, name calling, ignoring a consumer, threatening gestures, or refusing a consumer access to care or services as a means of punishment.
- Unexpected death – in the event of a fall, untreated pressure injury, or the actions of a consumer result in the death of another consumer.
- Stealing or financial coercion by a staff member – for example, if a staff member coerces a consumer to change their will to their advantage, or steals valuables from the consumer.
- Neglect – includes withholding personal care, untreated wounds, or insufficient assistance during meals.
- Inappropriate physical or chemical restraint – for example, where physical or chemical restraint is used without prior consent or without notifying the consumer’s representative as soon as practicable; where physical restraint is used in a non-emergency situation; or when a provider issues a drug to a consumer to influence their behaviour as a form of chemical restraint.
- Unexplained absence from care – this occurs when the consumer is absent from the service, it is unexplained and has been reported to the police.
Under SIRS, the Commission will be responsible for receiving all incident reports and will have the power to take regulatory action against any care providers found to have non-compliance.
The Commission will also have the power to issue notices for suspected non-compliance with SIRS requirements.
For more information, visit the SIRS page on the Commission’s website.
Find out how CarePage can support you to put in place the robust systems required under the SIRS.